BY Amr Youssef & Isabelle Devi Poirier
Sheradyne Prosper began experiencing mood swings in her mid-teens, cycling between extreme ‘highs’ and ‘lows.’ Initially dismissing these as typical adolescent changes, it was only as these emotional fluctuations became more intense and erratic that she sought answers.
“It’s like walking a tightrope, never knowing when I’ll lose my balance. Some days I’m filled with energy and optimism, but then it all comes crashing down,” says Prosper. “It’s a constant struggle, and it even started to impact my relationships, especially with my family.”
“I remember going to the emergency room, then being directed to the Douglas Mental Health University Institute, who then told me that I had to go back to another ER,” she says. “After two days of sitting in waiting rooms, all they did was prescribe me antidepressants that actually ended up giving me terrible side effects, and told me to get a referral from a family doctor, which I didn’t have.”

Douglas Mental Health University Institute, where Prosper was directed by the ER. Photo by Amr Youssef.
Going through the long process of seeking a psychiatrist or psychologist can intensify the burden that people with mental illness already face and make matters worse, according to Dr. Christine Grou, President of the Quebec Order of Psychologists. The process can also discourage them from continuing to seek help.
“If you want to see a psychologist in Quebec, you have two ways,” says Grou. “If you go by yourself and you have the money, you can go to a private practitioner, but if you want to go through the public healthcare system, then you’ll have to see your family physician who will assess and refer you, but the accessibility is still not necessarily easy.”
In Montreal, seeking the expertise of a psychiatrist requires an initial referral from a physician, followed by an evaluation at a local CLSC (Centre Local de Services Communautaires). Grou believes the system could be streamlined.
“Do you really need a reference? Do you really need to see two professionals before seeing a psychologist or psychiatrist?” she asks. “I think the collaboration with family physicians and psychologists is very precious. But we need to do everything we can to improve accessibility as well as the services we offer the population.”
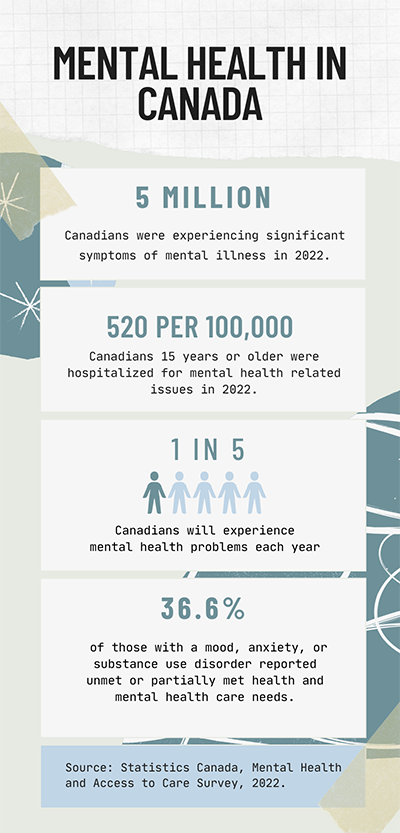
Quick facts about mental health in Canada. Infographic by Amr Youssef.
Post-evaluation, individuals are placed on a waiting list, which may span several months, before securing an appointment with a psychiatrist.
This process becomes even more complicated if one does not have access to a family doctor. According to a recent survey, the number of Canadians without a family doctor reached 6.5 million in 2023.
With wait times growing, some Montrealers are choosing to self-manage their treatment through alternative methods.
Medical Marijuana as an alternative treatment. Video by Isabelle Devi Poirier.
Choosing Wisely Quebec is an organization run by the Quebec College of Family Physicians (CQMF). It aims to reduce unnecessary tests and treatments in health care and to promote discussions between health-care professionals and their patients.
“One of the primary challenges we face is the deeply ingrained culture of ‘more is better’ in healthcare. Overcoming this mindset requires a shift in both clinical practice and patient expectations,” says Dr. Rene Wittmer, the president of Choosing Wisely. “Physicians sometimes prescribe tests and treatments that are not strictly necessary for various reasons.”
According to Wittmer, doctors may make decisions that may end up harming the patient or have them take unnecessary tests and medications due to the fast paced nature of health care.
“By focusing on appropriate and necessary interventions, we can streamline the diagnostic journey, reducing the time and resources spent on ineffective or redundant tests,” he explains. “We collaborate with health-care professionals and organizations to clarify diagnostic pathways and encourage the adoption of the best practices that reduce unnecessary interventions while ensuring patients receive the right diagnosis at the right time.”
Grou is optimistic the mental health care system can be improved through continued advocacy, education, and collaboration.
But there is a lot of work to do. Prosper only got her diagnosis when she found a family doctor after being on a waiting list for three years.
“I almost decided to give up and just live with it,” says Prosper. “I was tired of not being taken seriously because my case isn’t as severe as other people who may have attempted suicide, self harm or have any life-threatening condition. Some doctors really made me question my own symptoms and whether or not it was all just in my head.”




